01 Pages : 1-13
Abstract
Telehealth provides medical treatment, patient education, self-care, and health information using digital communication technology. Telehealth involves remote data exchange between a patient and a healthcare provider. Telehealth may enhance health care in underdeveloped countries. This research examines how Pakistani physicians and nurses see telemedicine for cardiovascular disease therapy. We employed non-probability sampling to pick respondents for this quantitative investigation. In this research, 30 individuals completed a well-designed questionnaire. 63% were male, 37% female. The researchers concluded that telemedicine intervention is useful for cardiovascular disease and possibly many other illnesses and ailments. These findings did not prove it was always useful. International NGOs are helping telehealth expand. These organisations help poor rural Pakistanis improve their health. Telehealth and personal health information has spread via electronic and social media. Telehealth helps battle cardiovascular problems by connecting patients in urban and rural Pakistan to competent hospitals and institutes. Telehealth may reduce patient wait times. Telehealth platform users who continuously address their particular health challenges may outperform the overall population, according to the research. Telehealth make treatment easier and more accessible for patients. There aren't enough physicians, nurses, hospital beds, specialists, or appointments on patients' chosen
Key Words
Telehealth, Telemedicine, Tele-clinic, health, Cardiovascular Diseases
Introduction
According to the definition provided by Telehealth | NEJM (2017), telehealth is the process of electronically transmitting health-related information from one location to another with the intention of delivering or improving medical treatment. Telehealth may also be referred to by its alternate name, which is telemedicine. The management of public health, the education of medical professionals, and the provision of clinical treatment may all be accomplished via the use of telehealth, which makes use of digital information and communications networks.
Telehealth is the use of a technologically mediated virtual platform to facilitate the delivery of necessary medical intervention, clinical and non-clinical services, participation in patient monitoring, reduction in the risk of medical complications, and dissemination of health information. When we talk about "telehealth," we are referring to the use of a technologically mediated virtual platform (Mechanic et al., 2021). The term "telehealth" refers to both the provision of medical treatment at a distance as well as the practise itself. The term "telehealth services" refers to a broad range of healthcare delivery methods, some of which include telepharmacy, telemedicine, and telemonitoring, as well as the delivery of healthcare services through mobile and desktop applications.
According to Metzger (2017), there is a paucity of research that investigates the effectiveness of telemedicine in the management of patients who suffer from cardiovascular diseases (CVDs). But even with this little data, we may be able to make key conclusions about the ways in which telehealth might be utilised to prevent, manage, and treat cardiovascular issues. He did this as part of a quantitative study in which he evaluated the satisfaction levels of patients with congestive heart failure who were treated at home with and without the use of telehealth. The results of statistical study conducted on the subject have indicated that when telehealth is used, older citizens are more satisfied with the medical care they get at home. The chance of a person getting an evaluation at an early stage increases when preventative measures are taken, as does the possibility that they will limit their exposure to risk factors such as smoking and high blood pressure. (Castro & Sawatzky, 2018 ).
Nasir et al., (2020) conducted research to investigate the variables that influence the dissemination and adoption of electronic health platforms in refugee settings in developing nations. They stated that the use of this technology might potentially assist enhance the health status of refugees. However, they also discovered a great deal of resistance in the form of a variety of obstacles, such as a lack of internet connectivity and the skills required to operate the programme. This conclusion was confirmed by Mitchell-Gillespie et al., (2020), who noted that the introduction of Telehealth had demonstrably successful outcomes in the near term. Obeidat et al., (2021) also argued that it is necessary to create a comprehensive national Telehealth strategy based on the effectiveness of several Telehealth initiatives, particularly in the midst of the COVID-19 epidemic. According to Khader et al. (2014), the use of telehealth in geographically dispersed areas has the potential to improve the quality of life, diagnosis, and intervention, as well as address challenges linked to access to health care treatment.
Rational
Pakistani hospitals rarely used telemedicine for
cardiovascular disease prevention, diagnosis, treatment, and management. Woo and Dowding (2018) found strong opposition to telemedicine. Telehealth or cardiovascular disease treatment is widely recognised, according to studies (Battineni et al., 2021). After critical care, these patients are often readmitted to hospitals. Hospital readmissions are high. The predicted 1 million Americans with cardiovascular disease will likely increase (Balbay et al., 2018). Hospital readmissions are costly. If nothing is done to resolve the issue of telemedicine's effectiveness in treating cardiovascular diseases, the quality of life of persons with cardiovascular diseases will continue to decline. Study is needed now more than ever since the major COV19 prevention strategy nationwide is social distancing. Telehealth services are growing as a result.
Telehealth programmes will educate more patients. Pakistan hasn't done enough study on telehealth's genuine utility, possible barriers, and other issues that affect its acceptance. Pakistan lacks research. Therefore, it is important to conduct research on the experiences of individuals and healthcare professionals who have interacted with the Telehealth system to deliver care to determine the system's efficacy at hospitals among patients and practitioners to solve Pakistan's telehealth programme challenges. This will help resolve Pakistan's challenges.
Research Question/Aim
1: How do physicians, nurses, and other healthcare professionals see telehealth's usefulness in treating cardiovascular diseases?
Research Objective
i. To examines healthcare workers' opinions on telehealth's effectiveness in managing major health issues.
ii. To learn more about the challenges faced and possible rewards of telehealth in Pakistan.
iii. To provide suggestions for methods to enhance the efficiency of telehealth and to make suggestions for ways to regulate it.
Literature Review
A number of different cardiac disorders, such as angina, heart attacks, congenital heart disease, and other heart conditions, are just some of the numerous medical issues that might have an impact on your health. The most obvious symptoms are discomfort in the chest, shortness of breath, nausea, heavy perspiration, and a racing heart. Indigestion, resistance to physical activity, and discomfort in the chest, back, and upper abdomen are only some of the symptoms that may be brought on by a wide range of disorders. In children, potential symptoms of heart disease include a light grey or blue complexion, swelling of the legs or belly, trouble breathing while eating, and sluggish or stunted growth. In adults, heart disease is the leading cause of death in the United States. There is also the possibility that other variables contribute to an increased risk of cardiovascular disease. Hypertension is the most common reason for high blood pressure in the arteries and veins, which in turn has an impact on the pace at which the heart beats and the overall health of the cardiovascular system.
Rehan et al., (2016) conducted research on a wide variety of possible cardiovascular disease (CVD) risk factors. Tobacco use, elevated cholesterol levels, diabetes, inadequate physical exercise, excess body fat, and a family history of cardiovascular disease were all factors that increased the likelihood of an individual developing cardiovascular disease. Patients, communities, and healthcare systems all across the world are all beginning to feel the weight of the immense load that long-term cardiovascular disease has imposed upon them. Multiple programmes with the goal of lowering the risk of cardiovascular disease have been linked to a decrease in the prevalence of cardiovascular illness. This is the reason why there have been so many developments in digital technology, such as telehealth, mobile phone apps, tablet apps, and computer programmes, to provide venues for the provision of venues for the provision of venues for the provision of flexible, low-cost, and easily accessible treatments for cardiovascular care. Telehealth programmes have shown to be quite beneficial throughout the course of recent years in the management and treatment of cardiovascular conditions.
Patients and medical professionals may communicate with one another via video conversations and wireless networks using telehealth services. It is used for things like keeping track of medication refills and lifestyle modifications as well as controlling prospective hazards. Additionally, it is used for managing potential risks. Patients suffering from cardiovascular disease are given the opportunity to monitor their symptoms and vitals via the use of telehealth, which ultimately results in better health outcomes and lower overall healthcare expenses. Estimates of physiologic data that may be obtained from home, such as a patient's heart rate, blood pressure, and blood sugar levels, may be sent on a regular basis to medical professionals. This makes it easier to keep track of patients' chronic diseases and to adjust therapy to the particulars of each individual's circumstance. Patients may now monitor their risk factors for cardiovascular disease and take responsibility of their own treatment thanks to developments in telehealth technology, which has allowed them to do so from a distance. This demonstrates how this technology has the potential to revolutionise the healthcare system by lowering the mortality rate of patients who suffer from cardiovascular disease and raising the level of care that is provided to patients and the families of those patients (Pekmezaris et al., 2019).
Barriers while Using Telehealth
The implementation of telehealth in impoverished nations such as Pakistan has a number of challenges, including cultural acceptability and knowledge, a lack of resources, political stability, inconsistency in health policy (which may vary from government to government), and technological difficulties. It is hypothesised that the lack of familiarity with telehealth technology is a major barrier to its implementation in developing countries, leading to a lack of interest on the part of both patients and doctors. This is due to the fact that patients and doctors are unable to communicate effectively with one another. Even though political stability and inconsistency in health policy are the most significant challenges, they are not insurmountable obstacles and may be solved by increasing knowledge, training the workforce, and overcoming barriers of culture and technology. It's possible that using the sorts of technologies that aren't widely used might make personal finance management easier (Hussain Jaifi Bahloul, 2014). Candidates who are qualified to participate in telehealth consultations need to be chosen. Patients whose diseases pose a significant risk to their lives are required to be sent to the hospital for treatment (Clerkin K J et al. 2020). The research papers that were looked at for this analysis included participation from doctors and other medical professionals working in a broad variety of specialties. To provide just one example, eight different studies included both medical professionals and nursing staff in their telehealth services (AlAzab & Khader, 2015; Blinkhorn, 2021).
The majority of the studies that were considered depended on the assistance of registered nurses for tasks such as the distribution of questionnaires. According to the findings of one research, community-based rehabilitation professionals may have participated in telehealth treatments (Bria Mitchell-Gillespie, 2020). According to the findings of one research, international specialists from UNRWA were providing assistance to the Jordanian Department of Refugees in the deployment of telehealth therapy (Nasir et al., 2020).
Telehealth Interventions in Managing Disease
Age, lifestyle, and hypertension raise heart disease
risk. Addressing even one risk improves treatment response. Rural places have a greater cardiovascular disease risk than cities (Lindroth et al., 2014). Telehealth-based interventions, according to the Journal of Rural Health, were the most effective way to treat cardiovascular disease in rural areas (Villarreal and Berbey-Alvarez). Telehealth programme developers concluded this (2020). Over half of hospitalised patients were readmitted within a few months, and rural areas had higher chronic disease death rates due to distance (CDC, 2016). Carefully monitor outpatient treatment programmes. Telehealth helps monitor patients remotely. Telemedicine patients had a decreased readmission rate (PubMed, 2015). Randolph et al., (1999) examined how telemedicine services may improve paediatric cardiovascular diagnosis and care. 1999 subset analysis of a bigger research. Telemedicine allows clinicians to screen babies and detect congenital neonatal diseases from home. Telehealth in a cardiology practise improved the clinic's attitude toward remote patients and its global outreach to cardiologists in low-income countries. The study used telehealth (Olatinwo, 2019).
Research Method
Interviews and fieldwork dominate the research. Exploratory research is recommended to determine the topic's importance and the study's main problem. Research will establish strong linkages and correlations (Abutabenjeh & Jaradat, 2018). Nasir et al. (2020) examined refugee mobile health distribution and uptake using an experimental strategy.
Quantitative research would help the suggested study acquire more data and give objective facts in numerical and statistical form. This inquiry may provide insight on its intended issue due to objective data. Quantitative methods provide in-depth case examination for enhanced understanding (Verhoef and Casebeer, 1997). Quantitative methods are best for determining if telehealth treats cardiovascular conditions, according to patients and healthcare experts (Wade et al., 2016).
The study's purpose is to gather insight through monitoring participants in their daily activities, so researchers may track the population of interest in its natural setting. This strategy lets researchers examine the population in its natural environment (Thanh & Thanh, 2015). This study seeks to capture the true thoughts, emotions, and experiences of Telehealth therapy participants. This research examined this objective quantitatively. The investigator's capacity to use open-ended questions and adapt them to explore the topic and find specifics is crucial to research.
Sampling
The researcher believes that the non-probability technique is superior than the probability method when it comes to picking the appropriate sample size. When using a non-probability sampling approach, researchers have the option of selecting a sample size based on their own discretion rather than on the output of a random number generator. If you are acquainted with the concept of probability sampling, then you will be aware that this strategy is in direct opposition to it. Researchers have more discretion in establishing sample sizes when they use non-probability sampling, so the results of their studies may be adjusted to meet the particular requirements of their investigation (Marshall 1996). The sample consists of thirty healthcare professionals (doctors, nurses, and others) who are simple to get in touch with. In order to take part at the study, participants are required to have prior experience with telemedicine and to either now work or have previously worked in a medical facility that specializes in treating heart disease.
Recruitment of Participants
A questionnaire gather the necessary data. This
questionnaire has closed-ended questions. The questionnaire asks about responder information, research, and digital health ethics. Twenty-five doctors and five nurses from cardiac hospitals and research organizations were selected for the study. This study's participants have experience using telemedicine to treat cardiovascular illness.
This inquiry began with a preliminary questionnaire test, which was utilized to improve the questionnaire. The health and technology-savvy core project team receives the research questionnaire when it is completed. Due to this rule, individuals with at least two years of experience will be considered.
Source of Data
In this research thirty responses with experience in a variety of hospitals and healthcare institutions and telemedicine services would be best. Participants in the research checked "yes" on a questionnaire section. This research analyzed healthcare workers' online questionnaire replies.
Demographic
As can be seen in the table that follows, those who worked in the health care industry and took part in the survey included 19 men and 11 females. In order to successfully complete the interview, it was necessary to get separate replies from each of them.
Table 1
|
S. No |
Female |
Male |
|
1 |
11 |
19 |
Female participation is 37%, shown by the red color in Figure-1, while the ratio of males is 63%, led by the blue color the below figure-1, participated in this study.
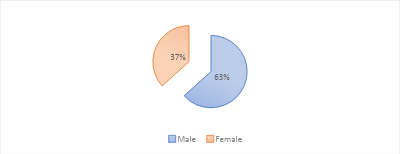
Table 2
Experience
|
Experience |
Female |
Male |
|
Two Years |
1 |
2 |
|
Three Years |
4 |
3 |
|
Four Years |
2 |
5 |
|
Five Years |
2 |
4 |
|
More than five years> |
2 |
5 |
|
Total |
11 |
19 |
During the interview, it was calculated that out of 30 respondents, two males and one female have two years of experience, as shown low table-2. Similarly, the male and four females had three years of experience, while five males had four years of field experience and two females with four years of experience. Similarly, out of 30 respondents, five males and two females were the most senior, all with five and more than five years of experience. As can be seen in the second table up from the bottom, there were at least three men and one female out of the thirty people who responded to the survey who had two years of experience. The one man and the four ladies combined their years of experience to make up three years, while the five men and two females combined their years of experience to make up four years. In a similar vein, out of the thirty people who participated in the study, the five males and two women who had the greatest experience were all five years old or older
Figure 2
Respondents Experience

The real experiences of the respondents are also shown in Figure 2, which will be covered in more detail later. The viewpoint of a female responder is represented by the colour red, whereas the perspective of a male respondent is represented by the colour blue. The blue tower at the very top indicates five males who know more than they're letting on, but the red tower at the very top represents three women who have four years of experience between them.
Table 3
|
Age |
Female |
Male |
|
24-34 |
2 |
3 |
|
34-44 |
5 |
5 |
|
44-54 |
3 |
9 |
|
54-64 |
1 |
2 |
|
Total |
11 |
19 |
Three guys and two women out of thirty young responders. 25–35 years old. As seen in table 3, two males and one woman were 55–65 years old.
Beneficial
Health care workers were given a questionnaire and questioned about their answers using their telehealth treatment expertise. Table 4 shows the factors in the first column and the professional's reply in the second. After calculation, each parent's financial aid is specified. Telemedicine therapy would help patients get care, according to 93% of study respondents. Telehealth also expands healthcare services, improving access and quality, respondents stated. 86.6% of respondents said telemedicine may improve patient health. Telehealth intervention saves money and time by avoiding hospital visits. Eighty-three percent of voters agree with this. Telemedicine intervention simplifies appointment scheduling for 83.33% of healthcare specialists. 86.33 percent of respondents felt that setting up a telemedicine session is easier and faster than setting up a person consultation, which may take a long time and is riskier.
Table 4
|
Benefits |
Percentage |
|
Expands access to medical & services. |
92.88 |
|
Delivers healthcare. |
87.85 |
|
Protects Traveling Time. |
84.55 |
|
Easy to get an appointment. |
84.44 |
|
As compared to in-person appointment Telehealth is easy and quick as. |
85.88 |
As demonstrates that patients benefit from telehealth therapy and have lower risk levels as a result. A horizontal cluster cone is also used to compare values in the different types of benefits depicted in Figure 4. The final cluster's horizontal cone is very long, suggesting that the usage of Telehealth significantly improves patients' access to medical care (by 93.33%, as shown by the cluster's strong response).
Figure 3

End of Use
As can see how the workers felt after their time with the product had come to an end in the table that follows (table 5). According to the data, over 80 percent of employees are of the opinion that medical experts are capable of swiftly picking up on how to use the Telehealth system. In addition, the fact that health professionals provide 86.66% of the responses shows how simple and straightforward it is for patients to utilize.
Table 5
|
End of Use |
Percentage |
|
For health professionals it is easy use Telehealth systems |
83.43 |
|
For patients Telehealth is easy to use |
85.55 |
Table 5 shows that the degree of risk among patients is related to the conclusion that telemedicine treatment is employed. The numbers in the table prove my point. Figure 5 provides additional explanation of the study's results by depicting a horizontal cluster cone that is used in evaluating relative worth among several types of advantages. Health professionals may see telehealth as simple to learn, as shown by the larger horizontal cone for the first cluster. The broader horizontal cone indicates that the majority of respondents (86.66 percent) agree with this statement. The data that are shown in Table 5 demonstrate that the conclusion that telemedicine treatment is employed is related to the amount of risk that is posed to patients. This is shown by the fact that the conclusion is offered in the table. My viewpoint is given more weight by the findings that are shown in the table. Figure 5, which illustrates a horizontal cluster cone, provides a detailed explanation of the results of the study. This explanation may be found below the figure. In the process of calculating the relative worth of the many different sorts of benefits, this particular kind of cone is used. The larger horizontal cone that represents the first cluster provides evidence that some individuals working in the health care business may have the perception that telemedicine is simple to understand. The wider horizontal cone illustrates that the majority of respondents (86.66 percent) agree with this statement, which means that they are in agreement
Figure 4

Results Discussions
Some early research suggests that there is great untapped potential in using telemedicine treatments in the treatment of cardiovascular problems in Pakistan. As a result, it is helpful to cultivate a network of healthcare specialists in Pakistan so that patients may obtain the therapy they need as soon as feasible. Also, this technology may be used to help new internal healthcare networks get off the ground and to promote the growth of public health systems that require assistance. In remote locations with developed telecommunications infrastructure, telehealth programmes have the ability to address long-standing difficulties in the delivery and coordination of high-quality medical care. This is feasible since internet access is often better in more remote locations. These programmes provide a viable alternative to the conventional means of delivering medical treatment and can be counted on to produce the desired results. We found that the satisfaction of a patient utilising telemedicine is influenced by a variety of different analytic topics. It was also observed that these motifs were predictive of patient satisfaction when utilising routine office visits. Based on the results of this research, patients' satisfaction with telehealth was affected when compared to their satisfaction with traditional in-office care. [Insert citation here] [Footnote required] Those who require a citation: In comparison to traditional medical treatments, telemedicine therapy greatly improved patient satisfaction in four categories. The results of this study suggest that patients are just as happy with telemedicine appointments as they are with traditional in-person checkups (if not more satisfied with in-office visits). This study's results were compared and contrasted with those from another similar examination that was conducted afterwards. These results from the study lend credence to the overall conclusions, which are described in further depth below. Research into the use of telehealth intervention in the treatment of cardiovascular diseases is urgently needed in light of these results, which emphasise the importance and utility of telehealth as an alternative means of delivering medical care. The level of attention provided is on par with that which one would get during a regular doctor's visit. Because of this, it is crucial to find methods to make it easier for senior citizens to access health-related information on the internet. The extent to which a person can understand the information being conveyed to them must be taken into account at every stage of the process and the creation of the product. Special consideration should be given to the user experience and the role of health responsibility in enticing the elderly to connect with and continue to utilise telehealth and online health information services. Learning more about the needs of older people in the context of the broader social context in which they find themselves, including the negative effects of dependence on children, necessitates research into the cultural biases that influence their decisions when using telehealth and online health information services, among other things. The expansion of the health sector in developing countries like Pakistan is hampered by a number of factors, including political instability, cultural barriers, inadequate funding, unstable infrastructure (such as reliable electricity, reliable internet access, and telehealth-capable devices), and contradictory health policies. Compared to metropolitan areas, rural areas have it far worse when it comes to these problems. The establishment of telemedicine clinics in Pakistan's rural and outlying areas is the focus of international partnership. The target demographic for these clinics consists of low-income patients with cardiac issues who would benefit from receiving treatment, advice,and resources in the comfort of their own home.
References
- Abdel-Razeq et al., .(2015). Recruitment difficulties in a home telecare trial. Journal of Telemedicine and Telecare, 12(1_suppl), 26– 28.
- Al-Samarrie et al. (2020). Effect of telehealth on use of secondary care and mortality: findings from the Whole System Demonstrator cluster randomised trial. BMJ, 344(jun21 3), e3874–e3874.
- Al-Zaytoonah. (2015). Systematic Literature Review on the Spread of Health-related Misinformation on Social Media. Social Science &Amp; Medicine, 240, 112552.
- Andersen, I. C., Thomsen, T. G., Bruun, P., Bødtger, U., & Hounsgaard, L. (2017). Patients’ and their family members’ experiences of participation in care following an acute exacerbation in chronic obstructive pulmonary disease: A phenomenological- hermeneutic study. Journal of Clinical Nursing, 26(23–24), 4877–4889.
- Balbay, Y., Gagnon-Arpin, I., Malhan, S., Öksüz, M. E., Sutherland, G., Dobrescu, A., & Habib, M. (2018). Modeling the burden of cardiovascular disease in Turkey. Anatolian Journal of Cardiology, 20(4), 235.
- Battineni, G., Sagaro, G. G., Chintalapudi, N., & Amenta, F. (2021). The Benefits of Telemedicine in Personalized Prevention of Cardiovascular Diseases (CVD): A Systematic Review. Journal of Personalized Medicine, 11(7), 658.
- Bhatt, M., & McElrath, (2020). Telemedicine: an unfruitful experience of tele-expertise in nephrology. Europe PMC, 112-116.
- Blinkhorn, (2020). When trust is not enough: a serial mediation model explaining the effect of race identity, eHealth information efficiency, and Information behavior on intention to participate in clinical research. Health Educ Behav.45(6), 1036–42.
- Bria, Mitchell-Gillespie. (2020). From solving a health problem to achieving quality of life: redefining eHealth literacy . J Literacy Technol. 2015, 16(2), 33–54.
- Castro & Sawatzky, (2018). Cardiovascular disease risk and prevention amongst Syrian refugees: mixed methods study of Médecins Sans Frontières program in Jordan. Conflict and Health.Retrieved April 27, 2021,
- CDC .(2019). CDC.
- Clerkin, K. J., et al. (2020). Media health literacy, eHealth literacy, and the role of the social environment in context. Int J Environ Res Public Health. 15(8), 1643.
- Combi, C., Pozzani, G. and Pozzi, G. (2016). Telemedicine for Developing Countries.
- Evans, R. S. (2016). Electronic health records: then, now, and in the future. Yearbook of medical informatics, (Suppl 1), S48.
- Hanlon, P., Daines, L., Campbell, C., McKinstry, B., Weller, D., & Pinnock, H. (2017). Telehealth Interventions to Support Self- Management of Long-Term Conditions: A Systematic Metareview of Diabetes, Heart Failure, Asthma, Chronic Obstructive Pulmonary Disease, and Cancer. Journal of Medical Internet Research, 19(5), e172.
- HosamAl-Samarraie et al., .(2020). User Acceptance of Information Technology: Toward a Unified View. MIS Quarterly, 27(3), 425.
- Hoti, K., Hughes, J. D., & Emmerton, L. (2014). Dr Google and the consumer: a quantitative study exploring the navigational needs and online health information-seeking behaviors of consumers with chronic health conditions.
- Hussain, J. B. (2014). National library of medicine current bibliographies in medicine: health literacy. Bethesda: National Institutes of Health;
- Islam, S. & Maddison, R. (2021). Digital health approaches for cardiovascular diseases prevention and management: lessons from preliminary studies.
- Jaber et al., .(2014). Cost-effectiveness of telehealth for patients with raised cardiovascular disease risk: evidence from the Healthlines randomised controlled trial. BMJ Open, 6(8), e012352.
- Jiang Y, Liu F, Guo J, Sun P, Chen Z, Li J, et al. (2020). Evaluating an intervention program using WeChat for patients with chronic obstructive pulmonary disease: a randomized controlled trial. J Med Internet Res.22(4), e17089.
- Khader, Y. S., Jarrah, M. I., Al-Shudifat, A. E. M., Shdaifat, A., Aljanabi, H., Al-Fakeh, S. I., Turk, E. E., Zayed, K. A., Al Quran, H. A., Ellauzi, Z. M., & Al Tahan, M. (2014). Telecardiology Application in Jordan: Its Impact on Diagnosis and Disease Management, Patients’ Quality of Life, and Time- and Cost-Savings. International Journal of Telemedicine and Applications, 2014, 1–6.
- Lee. (2020). Telemedicine Opportunities and developments in Member States.
- Levy, H., Janke, A. T., Langa, K. M .(2015). Health literacy and the digital divide among older Americans. J Gen Intern Med. 30(3), 284–9.
- Lindroth, M., Lundqvist, R., Lilja, M., & Eliasson, M. (2014). Cardiovascular risk factors differ between rural and urban Sweden: the 2009 Northern Sweden MONICA cohort. BMCPublic Health, 14(1).
- Marshall, M. N. (1996). Sampling for quantitative research. Family practice, 13(6), 522-526. Mechanic, O.J., Persaud, Y. and Kimball, A.B. (2021). Telehealth Systems. [online] PubMed.
- Metzger, L.M. (2017). Are patients satisfied with Telehealth in home health care? a quantitative research study in congestive heart failure patients. SM Gerontology and Geriatric Research, 1(2), 1009
- Mitchell-Gillespie, B., Hashim, H., Griffin, M., &AlHeresh, R. (2020). Sustainable support solutions for community-based rehabilitation workers in refugee camps: piloting telehealth acceptability and implementation. Globalization and Health, 16(1), 1-14
- Nasir, S., Goto, R., Kitamura, A., Ballout, G., Hababeh, M., Kiriya, J., Jimba, M. (2020 ). Dissemination and implementation of the e- MCH Handbook, UNRWA’s newly released maternal and child health mobile application: a cross sectional study. BMJ Open
- Obeidat, A. Z., & El-Salem, K. (2021). A national telemedicine program in the Kingdom of Jordan–Editorial
- Olatinwo. (2019). Telecardiology during the Covid-19 pandemic: past mistakes and future hopes. American Journal of Cardiovascular Disease, 10(2), 34.
- Pekmezaris, R., Nouryan, C. N., Schwartz, R., Castillo, S., Makaryus, A. N., Ahern, D., & DiMarzio, P. (2019). A randomized controlled trial comparing telehealth self- management to standard outpatient management in underserved black and Hispanic patients living with heart failure. Telemedicine and e-Health, 25(10), 917-925
- Qaddoumi et al., .(2008). Social support, health literacy, and health care utilization among older adults. Asia Pac J Public Health. 31(4), 359–66.
- Rehan et al. (2016). Empirical studies assessing the quality of health information for consumers on the world wide-web: a systematic review. Jama. 287(20):2691–700.
- Schoonenboom & Johnson .(2017). Telehealth in the developing world: current status and future prospects.
- Scott, K. C., Karem, P., Shifflet,t K., Vegi, L., Ravi, K., & Brooks, M. (2018). Evaluating barriers to adopting telemedicine worldwide: a systematic review. J Telemed Telecare.24(1):4–12
- Selzler, A. M., Wald, J., Sedeno, M., Jourdain, T., Janaudis-Ferreira, T., Goldstein, R., et al. (2018). Telehealth pulmonary rehabilitation: a review of the literature and an example of a nationwide initiative to improve the accessibility of pulmonary rehabilitation. Chron Respir Dis. 15(1):41–7.
- Shaw, T, McGregor D, Brunner, M., Keep, M., Janssen, A., & Barnet, S. ( 2017). What is eHealth (6)? Development of a conceptual model for eHealth: quantitative study with key informants . J Med Internet Res.19(10), e324.
- Thanh., & Thanh, (2015). Health literacy and the digital divide among older Americans. J Gen Intern Med. 30(3):284–9.
- Villarreal., & Berbey-Alvarez .(2020). Cardiovascular disease risk and prevention amongst Syrian refugees: mixed methods study of Médecins Sans Frontières programme in Jordan. Conflict and Health.
- Wade, V., Barnett, A. G., Martin-Khan, M., & Russell, T. (2016). Designing quantitative telemedicine research. Journal of Telemedicine and Telecare, 23(9), 786–791.
- Woo, K., & Dowding, D. (2018). Factors Affecting the Acceptance of Telehealth Services by Heart Failure Patients: An Integrative Review. Telemedicine and E-Health, 24(4), 292–300.
- Zhang, Y., Sun, Y., & Xie, B. (2015). Quality of health information for consumers on the web: A systematic review of indicators, criteria, tools, and evaluation results. Journal of the Association for Information Science and Technology, 66(10), 2071–2084.
- Zhang, Y., Zhang, H., Yang, Z., Sun, J., & Tan, C. D. (2019). Snowball Effect of User Participation in Online Environmental Communities: Elaboration Likelihood under Social Influence. International Journal of Environmental Research and Public Health, 16(17), 3198.
Cite this article
-
APA : Arif, I. (2022). Telehealth Intervention of Cardiovascular Diseases Patients: A Quantitative Study. Global Drug Design & Development Review, VII(IV), 1-13. https://doi.org/10.31703/gdddr.2022(VII-IV).01
-
CHICAGO : Arif, Irfan. 2022. "Telehealth Intervention of Cardiovascular Diseases Patients: A Quantitative Study." Global Drug Design & Development Review, VII (IV): 1-13 doi: 10.31703/gdddr.2022(VII-IV).01
-
HARVARD : ARIF, I. 2022. Telehealth Intervention of Cardiovascular Diseases Patients: A Quantitative Study. Global Drug Design & Development Review, VII, 1-13.
-
MHRA : Arif, Irfan. 2022. "Telehealth Intervention of Cardiovascular Diseases Patients: A Quantitative Study." Global Drug Design & Development Review, VII: 1-13
-
MLA : Arif, Irfan. "Telehealth Intervention of Cardiovascular Diseases Patients: A Quantitative Study." Global Drug Design & Development Review, VII.IV (2022): 1-13 Print.
-
OXFORD : Arif, Irfan (2022), "Telehealth Intervention of Cardiovascular Diseases Patients: A Quantitative Study", Global Drug Design & Development Review, VII (IV), 1-13
-
TURABIAN : Arif, Irfan. "Telehealth Intervention of Cardiovascular Diseases Patients: A Quantitative Study." Global Drug Design & Development Review VII, no. IV (2022): 1-13. https://doi.org/10.31703/gdddr.2022(VII-IV).01
