Abstract
People with epilepsy often have between 30 and 50% of their patients with neuropsychiatric disorders. The major neurological comorbidities linked with epilepsy, such as migraine, dementia, traumatic brain injury, and autism spectrum disorder, have relative effects on some of the psychiatric disorders, such as mood and anxiety disorders. The current research objective was to report the usage of pharmacologic drugs in the treatment of a neuropsychiatric disorder in epilepsy. A total of 630 patients of different aged groups (9-18 years, between 19-64 years and Elderly > 65 years) were included in our research. The study was carried out at Qazi Hussain Ahmed Medical Complex Nowshera from September 2021 to Jan 2022. Epilepsy patients in rural areas had a substantially lower incidence of neuropsychiatric disorders than those in urban areas, and most of the patients were men. The most often used Anti epilepsy drugs (AEDs) for treating epilepsy were lamotrigine, valproate, and levetiracetam, which were used by 50% of participants. Carbamazepine was only used by adults and was least frequently utilized by older people. In order to effectively manage neuro-psychiatric comorbidities in epilepsy, it is important to consider both possible iatrogenic and therapeutic consequences.
Key Words
Psychiatric & Neurological Comorbidities, Epilepsy, Neuropsychiatric Disorders
Introduction
People with epilepsy (PWE) tend to have neuropsychiatric disorders, which typically impact 20–40% of patients. Community studies have demonstrated a 37% lifetime incidence of psychological disorders in these individuals, with the majority being anxiety and mood issues; within neurological disorders, migraines are the most frequent, with incidence rates of 20–40%. When preparing a strategy for the therapy of any seizure disease, it is important to take into account the complicated link between epilepsy and neuropsychiatric abnormalities. A few of the prevalent neurological disorders linked to epilepsy and some psychiatric diseases frequently co-occur . Patients with such foremost psychotic illnesses, such as attention deficit-hyperactivity disorder (ADHD) and mood, anxiety, and psychotic disorders, are already at greater risk of developing epilepsy and neurological illnesses. A thorough therapeutic approach in any PWE must properly examine and manage neurological and psychiatric problems in addition to striving towards seizure-free conditions [10]. Nevertheless, a lot of challenges typically stand in the way of such thorough administration. The management of neurophysiological comorbidities is frequently overlooked in the therapeutic process for a seizure disorder; the treatment of psychiatric comorbidities is empirical as data based on scientifically valid investigations are lacking, and psychiatric comorbidities are frequently undiagnosed. The administration of mental disorders in PWE has been hampered by a number of misunderstandings regarding the "reported proconvulsant effects" of psychotropic medications, and seizure disorders can be adversely affected by medications and medical techniques used to address them.
The current research objective was to report the usage of pharmacologic drugs in the treatment of a neuropsychiatric disorder in epilepsy.
Material and Methods
The study was carried out at Qazi Hussain Ahmed Medical Complex Nowshera from September 2021 to Jan 2022, Pakistan. A total of 630 patients of different aged groups (9-18 years, between 19-64 years and Elderly > 65 years) were included in our research. To evaluate disparities comparing PWE living in urban regions and those who reside in rural areas, we additionally classified our study of epilepsy depending on the amount of urbanization. Written informed consent was signed and proper counselling was done. A detailed clinical history and examination of all cases were collected. The International Statistical Classification of Diseases (ICD-10) coding system, specifically the Psychological or Behavioral Diseases category, was used to organize the mental illnesses listed in the health records.
The beneficiary database was connected to the SQL Server 2013 software system using information from order forms and prescriptions. All data processing, including data selection, data merge, aggregation of data, and computations, was carried out using Microsoft Excel 2003 and SPSS, Version 17.0 software programmes. Our stratified evaluations of the frequency of epilepsy depending on age, gender, and amount of urbanization employed the chi-squared test. To calculate the odds ratios and 95% confidence intervals for the disorders and the degrees of urbanization, we analyzed the data for the groups of epileptic and non-epileptic patients. A statistically significant difference was determined to exist when the P value was less than 0.05.
Results
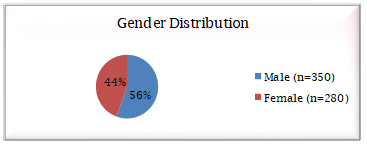
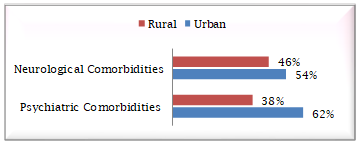
Out of the total of 630 patients, 280 (44.44%) were females and 350 (55.56%) were males (figure 1). Characteristics of the patients and seizure classification are shown in Table 1. Patients with epilepsy in rural regions had a dramatically lower frequency of psychiatric disorders compared to those in urban regions, and segmentation based on urbanization did not find a considerable variation in the general incidence of neurological disorders among patients having epilepsy (Graph 2).
Graph 1
Gender Distribution of Patients having Epilepsy
Figure 2
Division of Regions and the Neuro-psychiatric Comorbidities Incidence of Epilepsy Seizure
Table 1. Demographic
Characteristics of the Study Population
|
Characteristics
of the Study population |
Patients Number (Female/Male) (Percentage) |
|
Average age (years) |
41 (range: 8–92) |
|
Categories According to
Age |
|
|
9 to 18 years Old
Children |
167 (10 W/13 M)
(26.50%) |
|
9 to 64-year-old Adults
|
346 (58 W/48 M)
(54.92%) |
|
Elderly (65 to 90 years
old) |
117 (9 W/12 M) (18.58%) |
|
Classification of Seizures |
|
|
Generalized
tonic-clonic seizures |
123 (19.52%) |
|
Absence seizures |
41 (6.5%) |
|
Tonic, myoclonic, and
atonic seizures |
57 (9.04%) |
|
Complex partial
seizures |
93 (14.76%) |
|
Simple partial seizures |
23 (3.65) |
|
Psychogenic
non-epileptic seizures (PNES) |
83 (13.71%) |
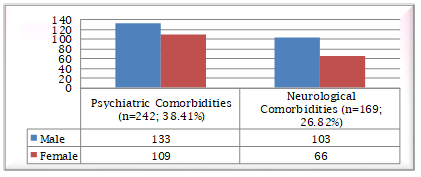
Among the 630
PWE, 242 participants (38.41%) had psychiatric disorders, of whom 109
individuals (45.04%) were women and 133 patients (54.96%) were male. Similarly,
169 patients (26.82%) had neurological comorbidities and of 169 patients, 103
patients were males (60.9%) and 66 patients were females (39.05%) (figure 3).
Learning impairment (34.29%), developmental delay (25.20%), mental retardation
(18.59%), ADHD 13.63%, and sleep problems (8.29%) constituted the most
prevalent psychiatric disorders in patients. Cerebral palsy (40.24%), head
injury (28.99%), congenital brain abnormalities (20.12%), and cerebral vascular
disease (10.65%) were the most prevalent neurological disorders (Table 2).
Graph 3
Epilepsy Patients having Psychiatric Comorbidities and Neurological Comorbidities
Table 2. Current
Research Identified the Major Disorders
|
Psychiatric
comorbidities |
Disorder |
Male |
Female |
Rate of
co-morbidity |
Odds ratio |
|
learning
disability |
44 |
39 |
34.29 |
32.3 |
|
|
developmental
delay |
33 |
28 |
25.20 |
18.4 |
|
|
mental
retardation |
24 |
21 |
18.59 |
9.3 |
|
|
attention
deficit hyperactivity disorder |
17 |
16 |
13.63 |
3.3 |
|
|
sleep
disorders |
15 |
5 |
8.29 |
6.1 |
|
|
Neurological
comorbidities |
Cerebral
palsy |
41 |
27 |
40.24 |
45.7 |
|
head injury |
30 |
19 |
28.99 |
22.3 |
|
|
congenital
brain anomaly |
21 |
13 |
20.12 |
17.6 |
|
|
cerebral
vascular disorder |
11 |
7 |
10.65 |
11.45 |
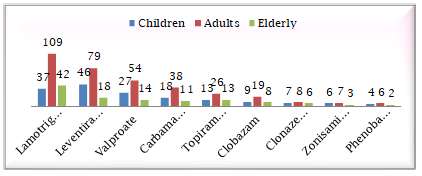
Lamotrigine,
valproate and levetiracetam were the mainly frequently used drug in epilepsy,
comprising 50 per cent of the patients due to better efficacy but having few
side effects. All age groups used lamotrigine. Levetiracetam was utilised by
both adults and children. Compared to carbamazepine, which was only used by
adults and was less commonly used by senior people over 65, valproic acid was
used by children and adults (Graph 4). Additionally, AEDs have beneficial
psychotropic effects that must constantly be taken into account when treating
neuro-psychiatric disorders in individuals with epilepsy (Table 3).
Graph 4
Antiepileptic Medicine use in People with Neuro-psychiatric Comorbidities, Including Children, Adults, and the Elderly Patients
Table 3. Antiepileptic
Drugs with Positive and Negative Psychotropic Properties
|
AED |
Psychiatric
benefits |
Neurological
benefits |
Side
Effects |
|
Lamotrigine |
Mood stabilizing Antidepressant |
control migraine and
seizures, |
§ dizziness § tired feeling |
|
Levetiracetam |
Anxiolytic |
control partial
seizures, myoclonic seizures, or tonic-clonic seizures |
§ Drowsiness § tired feeling,
|
|
Valproate |
Anxiolytic |
prevent migraine
headache |
nausea, asthenia, and
dizziness |
|
Carbamazepine |
Antidepressant |
Treat acute manic |
§
dizziness,
§
drowsiness,
§
and
vomiting |
|
Topiramate |
Mood stabilizing |
No |
§
mental
slowing, §
word-finding
difficulty, §
agitation
and irritability |
|
Clobazam |
Anxiolytic (generalized
anxiety disorder |
treatment of seizures
especially in children |
§
worsening
of depression, §
hallucinations |
|
Clonazepam |
No |
No |
§
drowsiness, §
dizziness, §
weakness, |
|
Zonisamide |
No |
control migraine |
agitated, irritable, or
display other abnormal behaviours |
|
Phenobarbital |
No |
Treat seizures, |
§
dizziness, §
drowsiness, §
problems
with memory or concentration |
Discussion
The rates of neuropsychiatric disorders, the incidence of epilepsy in patients of various ages, the differential between epilepsy in rural and urban areas, and the use of antiepileptic medicines (AEDs) in children, adults, and elderly epilepsy patients with neuro-psychiatric comorbidities are all included in this research. According to our research data, the percentage of male (n=350; 55.56%) who suffered from epilepsy were higher than female (n=280; 44.44%) this might be owing to men's occupation and their exposure to risk factors, such as head trauma and alcohol use. Additionally, because of the stigma and low family economic status in rural areas, females tend to have a lower consultation rate. These findings are similar to studies were done by Banerjee et al., (2009) and McHugh and Delanty (2008).
In our epilepsy population, the prevalence of mental and neurological comorbidities was not significantly impacted by urbanisation. However, individuals residing in rural locations are less likely to have mental comorbidities than those in metropolitan areas. According to research, rural regions had a much lower frequency and incidence of epilepsy with neuropsychiatric comorbidities, which is consistent with our findings. A possible explanation for this finding was the dearth of medical services for diagnosing paediatric mental issues in remote locations. In our research, 242 patients (38.41%) had psychiatric comorbidities and 169 patients (26.82%) had neurological comorbidities. Learning difficulty (34.29%) and developmental delay (25.20%) were the two most prevalent psychiatric comorbidities among epilepsy patients while cerebral palsy (40.24%), and head injury (28.99%) were the most common neurological comorbidities. These findings are similar to studies done by Chiang and Cheng (2014).
In our study, several AEDs were utilized to treat neurological and mental comorbidities in epilepsy patients. The most popular AEDs for treating epilepsy were lamotrigine, valproate, and levetiracetam, taken by 50% of patients. Levetiracetam was utilised in both children and adults, but Lamotrigine was used across all age groups. Compared to carbamazepine, which was only used by adults and was used less in the elderly; valproic acid was used by both children and adults and less in those over the age of 65. Patients with epilepsy who also had neuro-psychiatric comorbidities utilized almost identical AEDs.
Conclusion
In people with epilepsy, treating neuro-psychiatric comorbidities problems is a crucial concern. The research analyzed in this article demonstrates unequivocally that patients with epilepsy are more likely to have neurological and mental comorbidities. In order to effectively treat mental and neurological comorbidities in epilepsy patients, the pharmaceutical regimen must take into account both the potential therapeutic benefit and the adverse effects of AEDs.
References
- Banerjee, P. N., Filippi, D., & Allen Hauser, W. (2009). The descriptive epidemiology of epilepsy—A review. Epilepsy Research, 85(1), 31– 45.
- Breslau, N., Lipton, R. B., Stewart, W. F., Schultz, L. R., & Welch, K. M. (2003). Comorbidity of migraine and depression: Investigating potential etiology and prognosis. Neurology, 60(8), 1308– 1312.
- Chiang, K. L., & Cheng, C. Y. (2014). Prevalence and neuro-psychiatric comorbidities of pediatric epilepsy in Taiwan: A national population-based study. Epilepsy Research, 108(8), 1451– 1460.
- Chien, I. C., Lin, C. H., Chou, Y. J., & Chou, P. (2012). Prevalence, incidence, and stimulant use of attention-deficit hyperactivity disorder in Taiwan, 1996–2005: a national population-based study. Social Psychiatry and Psychiatric Epidemiology, 47(12), 1885– 1890.
- Devinsky, O. (2003). Psychiatric comorbidity in patients with epilepsy: implications for diagnosis and treatment. Epilepsy &Amp; Behavior, 4, 2– 10.
- Gaitatzis, A., Trimble, M. R., & Sander, J. W. (2004). The psychiatric comorbidity of epilepsy. Acta Neurologica Scandinavica, 110(4), 207– 220.
- Hesdorffer, D. C., LúðvÃgsson, P., Hauser, W. A., Ólafsson, E., & Kjartansson, L. (2007). Co- occurrence of major depression or suicide attempt with migraine with aura and risk for unprovoked seizure. Epilepsy Research, 75(2–3), 220– 223.
- Kanner, A. M. (2003). Depression in epilepsy: a frequently neglected multifaceted disorder. Epilepsy &Amp; Behavior, 4, 11– 19.
- Kanner, A. M. (2016). Management of psychiatric and neurological comorbidities in epilepsy. Nature Reviews Neurology, 12(2), 106– 116.
- Kanner, A. M. (2016). Management of psychiatric and neurological comorbidities in epilepsy. Nature Reviews Neurology, 12(2), 106– 116.
- Kanner, A. M. (2017). Psychiatric comorbidities in new onset epilepsy: Should they be always investigated? Seizure, 49, 79– 82.
- Kanner, A. M., & Balabanov, A. (2002). Depression and epilepsy: How closely related are they? Neurology, 58(Issue 8, Supplement 5), S27 S39.
- Karouni, M., Arulthas, S., Larsson, P. G., Rytter, E., Johannessen, S. I., & Johannessen Landmark, C. (2010). Psychiatric comorbidity in patients with epilepsy: a population-based study. European Journal of Clinical Pharmacology, 66(11), 1151– 1160.
- Larson, S. L., Owens, P. L., Ford, D., & Eaton, W. (2001). Depressive disorder, dysthymia, and risk of stroke: thirteen-year follow-up from the Baltimore Epidemiological Catchment Area Study. Stroke 32, 1979– 1983.
- Laxer, K. D., Trinka, E., Hirsch, L. J., Cendes, F., Langfitt, J., Delanty, N., Resnick, T., & Benbadis, S. R. (2014). The consequences of refractory epilepsy and its treatment. Epilepsy &Amp; Behavior, 37, 59– 70.
- Lopez, M. R., Schachter, S. C., & Kanner, A. M. (2019). Psychiatric comorbidities go unrecognized in patients with epilepsy: “You see what you know.†Epilepsy &Amp; Behavior, 98, 302– 305.
- McHugh, J. C., & Delanty, N. (2008). Epidemiology and classification of epilepsy: gender comparisons. International review of neurobiology, 83, 11-26.
- Stoyan Popkirov, Ali A. Asadi-Pooya, Roderick Duncan, David Gigineishvili, Coraline Hingray, Andres M. Kanner, W. Curt LaFrance, Chrisma Pretorius, & Markus Reuber. (2019). The aetiology of psychogenic non-epileptic seizures: risk factors and comorbidities. Epileptic Disorders, 21(6), 529– 547.
- Stephen, L. J., Forsyth, M., Kelly, K., & Brodie, M. J. (2012). Antiepileptic drug combinations—Have newer agents altered clinical outcomes? Epilepsy Research, 98(2– 3), 194– 198.
- Tellez-Zenteno, J. F., Patten, S. B., Jetté, N., Williams, J., & Wiebe, S. Psychiatric comorbidity in epilepsy: a population-based analysis. Epilepsia 48, 2336–2344 (2007).
Cite this article
-
APA : Mufti, A. A., Khan, M. K., & Khan, G. (2022). Management of Psychiatric and Neurological Comorbidities in Epilepsy. Global Drug Design & Development Review, VII(I), 18-25. https://doi.org/10.31703/gdddr.2022(VII-I).03
-
CHICAGO : Mufti, Ali Ahsan, Muhammad Kamran Khan, and Ghaazaan Khan. 2022. "Management of Psychiatric and Neurological Comorbidities in Epilepsy." Global Drug Design & Development Review, VII (I): 18-25 doi: 10.31703/gdddr.2022(VII-I).03
-
HARVARD : MUFTI, A. A., KHAN, M. K. & KHAN, G. 2022. Management of Psychiatric and Neurological Comorbidities in Epilepsy. Global Drug Design & Development Review, VII, 18-25.
-
MHRA : Mufti, Ali Ahsan, Muhammad Kamran Khan, and Ghaazaan Khan. 2022. "Management of Psychiatric and Neurological Comorbidities in Epilepsy." Global Drug Design & Development Review, VII: 18-25
-
MLA : Mufti, Ali Ahsan, Muhammad Kamran Khan, and Ghaazaan Khan. "Management of Psychiatric and Neurological Comorbidities in Epilepsy." Global Drug Design & Development Review, VII.I (2022): 18-25 Print.
-
OXFORD : Mufti, Ali Ahsan, Khan, Muhammad Kamran, and Khan, Ghaazaan (2022), "Management of Psychiatric and Neurological Comorbidities in Epilepsy", Global Drug Design & Development Review, VII (I), 18-25
-
TURABIAN : Mufti, Ali Ahsan, Muhammad Kamran Khan, and Ghaazaan Khan. "Management of Psychiatric and Neurological Comorbidities in Epilepsy." Global Drug Design & Development Review VII, no. I (2022): 18-25. https://doi.org/10.31703/gdddr.2022(VII-I).03